[Content Note: Health Issues, Heart Disease, Heart Failure, Needles]
Before yesterday, my last appointment with my cardiologist was last May. I’ve seen my GP a few times since then, as well as urgent care doctors when I’ve had a cold that lingered just a little too long for my tastes. So when my cardiologist reviewed my chart at the beginning of this week and saw that the doctors in internal medicine had been playing with my diuretics, He decided it was time to see me again now rather than waiting to the appointment I had scheduled for May.
I showed up at his office a few minutes after my appointment time, a bit frazzled. (A nasty accident on Elmwood turned what should have been a half hour drive to nearly an hour drive.) Needless to say, the stress of being late had my blood pressure up — even more than it normally is due to my penchant for white lab coat hypertension.
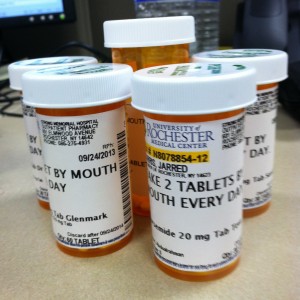
After the technician took all my vitals and got me seated comfortably in the exam room, my doctor came in less than five minutes later (the advantage of scheduling the early morning appointments is that they’re usually neither busy nor falling behind schedule yet). He asked me what was going on and I gave him a brief run-down, then gave me a brief exam. We talked a bit more and said I probably need to go for an echocardiogram since my last one was over a year ago. Also he noted the same symptoms they were seeing in internal medicine, so he said he was going to change my diuretic and double the dosage. Then he went to talk to the supervising doctor in the cardiology department.
The supervising doctor came back in the room — as is common — and talked to me some more, then asked me to hop back up on the exam table so he could take a look too. He checked me out and found the same symptoms every other doctor has found. However, he wasn’t eager to blame them on my heart. He noticed other signs that suggest that my heart may just be fine and pointed out that the symptoms I am exhibiting can be caused by other factors1. As such, he said he didn’t want to throw more diuretics at me without a definitive answer. So in addition to the echocardiogram — which he managed to get scheduled immediately after my visit in cardiology — he recommended a chest X-Ray (to determine if there actually is any fluid in my lungs) and some blood work. Which meant spending an hour or two hopping from department to department in the hospital.
Since it was right next door and is the only thing that had to be scheduled, I immediately went over to get the echocardiogram. That’s always a fun procedure, and this was my third time at it. Basically, you take off your shirt, lie on a bed and let the technician run an ultrasound probe all over your chest while fiddling with the controls. This time, though, the tech also took shots of my abdomen and throat, which was a new experience. I look forward to finding out what that was all about.
The hardest part of the echocardiogram is the contrast dye. They inject it into a vein to get better contrast in the images, which helps them take more accurate measurements. The put it in through an IV port. That means that — unless you have other tests scheduled that also require an IV port — they put one in, take about ten minutes to do that part of the procedure, and take it right back out.
After that, it was off to the outpatient lab to get blood drawn. They needed three vials this time. I joked about that to the phlebotomist and she responded, “Yeah, we only take as much as they need.” I told her that was good, as I kind of like my blood. I was also pretty impressed with the this phlebotomist. Not only did she manage to get blood with only one try, but I think it was the closest I’ve come to having blood drawn completely painlessly. (Well, other than the time in the hospital when I’m pretty sure I slept through the whole thing.) I barely even felt the needle.
After that, it was off to radiology for chest X-Rays. I was a bit concerned about how long that would take. When I had a chest X-Ray back in October, they were packed and it took them about half an hour to call me. Even then, they actually took me to a different part of the hospital because they were so backlogged. (I”m guessing this is probably why the radiology department validates parking for their patients.)
However, they were pretty slow yesterday morning. They called me in less than five minutes. After that, it was just a matter of posing for the nice woman, praying that the radiation would give me superpowers instead of cancer, and going on my merry way.
Now the hard part is waiting for my cardiologist to look over the results and call me back with answers. Fortunately, I’m able to see all my results (except for the echocardiogram) this morning. What I can see looks pretty good:
- My calcium and platelets are both low, but otherwise my blood work looks great.
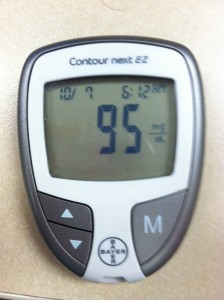
- My A1c (I was totally surprised when my cardiologist — who usually doesn’t care about my diabetes — ordered one) is a mere 6.0.
- The report from the chest X-Ray indicates that both my central airways and my lungs are normal. No mention of fluid, so I’m guessing that means there isn’t any. Sadly, it also doesn’t give any indication as to what’s causing the crackling sound in my lungs, which is what everyone panicking that my heart might be getting worse again.
So unless the echo shows something to be concerned about, this is probably a good indication that my heart is happy. Hopefully the cardiologist will be able to shed some more light on things whenever he calls.
And hopefully we can figure out what really is causing my symptoms so everyone will quit throwing diuretics at me until they’re actually necessary.
1This seems to be the problem with getting a diagnosis of something like congestive heart failure. If a symptom can be attributed to that diagnosis, most doctors are inclined to assume that’s what’s going on and act accordingly. That’s great if they’re right. If they’re wrong, you end up wasting a lot of time treating the wrong thing.