Hello dear readers! In the brief note at the top of my previous post, I mentioned that I’d be giving a bit of an update on my health situation. This post is that update. There’s going to be a lot of medical terms and links in this one, so buckle up!
I saw an electrophysiologist on the thirtieth of last month. To be honest, I had never heard of an electrophysiologist until my regular cardiologist told me he wanted to refer me to one back in October. I was surprised to learn there are specializations even within the specialization of cardiology.
I find it convenient that not only are my two cardiologists part of the same health group, but they actually work out of the same office. So finding Dr. Gallagher (my electrophysiologist) that day was pretty easy. Learning to remember all the medical terms he threw out during our visit took a bit of time. In fact, I had to google a couple of abbreviations he threw out to find/remember the full terms.
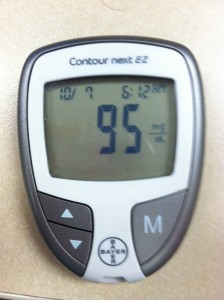
That Thursday was the first time I had heard anyone say the word supraventricular tachycardia (SVT), which is the definite diagnosis I currently have. Provisionally, Dr. Gallagher has given a further diagnosis of atrioventrucular nodal reentrant tachycardia (AVNRT), which is a specific category of SVT.1 According to sources I found online, it’s also the most common category of SVT. With that diagnosis, Dr. Gallagher moved on to discuss the possible courses of treatment.
The treatment that he recommends — and the one I eventually decided on — was to schedule an electrophysiology study (EPS) to find the “extra circuit” that he suspects is causing my SVT/AVNRT. If he can find it and he deems it sufficiently low-risk to do so, he will then effectively “break” that circuit with an ablation procedure. This could eventually cure my SVT/AVNRT.2 He says the probability that everything will work out that way are good (about 90%). The other 10% involves choosing an alternative treatment, either using medication or putting in a pacemaker.
The good news is that the EPS and ablation procedure can be done as an outpatient procedure. Sure, it’ll be an all-day stay at the hospital (I have to lay flat on my back for four hours and be monitored as they ensure the hole in the artery in my thigh closes up properly), but I should be able to come home and sleep in my own bed/recliner. The recovery is also pretty simple with restricted physical activity (in particular, lifting no more than ten pounds) for a week or less.
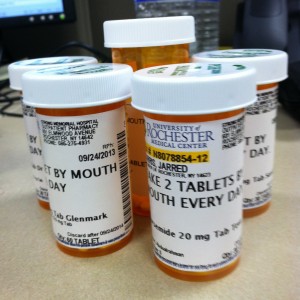
The only downside is there is a tiny chance (1% or less) of something going really badly. We’re talking heart attack and stroke territory. But like I said, that’s extremely unlikely. However, given that I have a husband who struggles with anxiety and was bound to get triggered as that part of his brain played out all those worst case scenarios, I did ask Dr. Gallagher to discuss the other most obvious option, which is treatment with medicine. Naturally, this is less desirable, as it’s a lifelong treatment rather than a potential cure. But Not causing my husband to experience any anxiety attacks seemed like something I might take another pill for the rest of my life for. I mean, I’m already up to six oral medications a day, a weekly injectible, and thrice daily insulin shots.
That approach ended up having it’s own problems. As Dr. Gallagher reviewed my chart, he realized the only medication he could potentially treat my SVT with was sotalol. Going on sotalol involves a two-night stay in the hospital for monitoring. A hospital stay was not going to help my husband’s anxiety either, especially since our local hospital doesn’t like to let family stay overnight.3 So I wasn’t sure what to do.
Fortunately, I didn’t have to make a decision that day and Dr. Gallagher agreed to just raise my dosage of of metoprolol while I came home and discussed the news and options with hubby.
In the end, I wasn’t able to help hubby avoid the anxiety attacks, but we got through them. And over the course of a few days, we decided to go with the EPS and potential ablation procedure. Ultimately we decided the idea of me coming home from the hospital the same day and the potential to just to cure the SVT outright was the better option, despite the risks. Especially when we considered just how low the risks are. Also, if I’m being honest, the thought of going on a medication that required me to stay in the hospital for monitoring made me uncomfortable. I haven’t researched it, but I find myself wondering just how harsh this medication is.
So after about a week of talking and letting things settle, I called and asked a few more questions. As part of that conversation, I informed the staff that I wanted to schedule the EPS/ablation procedure. They told me they’d send a message to Dr. Gallagher and get back to me with a potential date. And that’s what I’m waiting for now.
They did tell me that they’re booked out a ways and I’m probably looking at a date “sometime in the Spring.” This is fine with me, as I’d really like to get our vehicle back on the road. I’ve been taking Ubers everywhere (thank goodness I can work from home) and would prefer to change that so i don’t have to come home from the hospital in an Uber.
Fortunately, all my test results show that my heart is quite strong and healthy, so the delay is not a problem in that regard.4 Now the only reason to get it done as soon as possible is to get it over with so hubby can quit experiencing anxiety over it. And to be honest, I’m a bit nervous myself. I’ll be happy to put this in my rear-view mirror.
Post HIstory: This post was drafted. proofread, revised, and finalized on 8 February 2025.
Footnotes
- Dr. Gallagher’s assistant/student mentioned one other form of SVT, but I don’t remember what that was. Either way, the treatment moving forward seems to be the same. ↩︎
- Unfortunately, this will do nothing for my cardiomyopathy. That damage is permanent. But I can continue to manage that through my current regiment of medications. ↩︎
- Dr. Gallagher and I had already discussed my husband’s anxiety as we talked about the EPS and ablation procedure, so I asked him if there was anyway he could arrange for permission for him to spend the night with me. Unfortunately, he said he couldn’t guarantee that. This just further annoys me with our local hospital. ↩︎
- Granted, if my health were more critical, I’d like to think they’d find a way to fast-track my procedure. But the reality is that AVNRT is often not even something that needs to be treated. But given just how fast my heart beats when I have an episode, it’s time to do something about it in my case. ↩︎